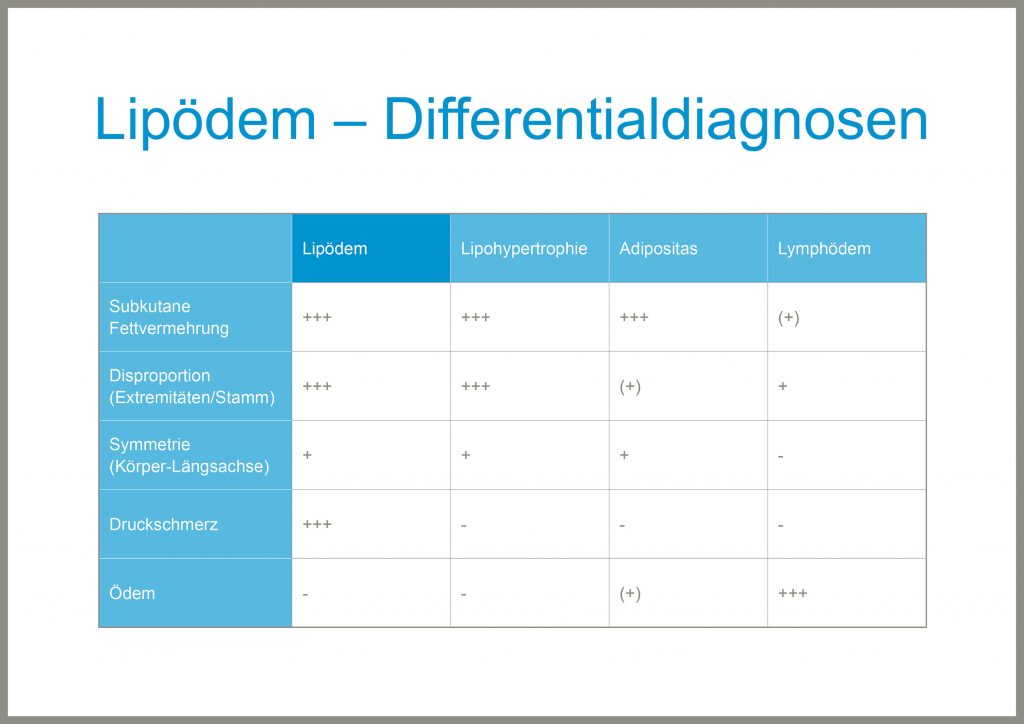
Lipedema (Greek: Lipos = fat / Oedem = swelling) is a chronic progressive disease of women, which is characterized by an abnormal distribution of fat. It is the result of symmetrical increase in subcutaneous fat on the legs and in up to 50% of the cases the upper arms also. In addition, the tissue tends to take up water and become swollen, and is easily bruised. Lipedema tissue is often tender to the touch or painful.
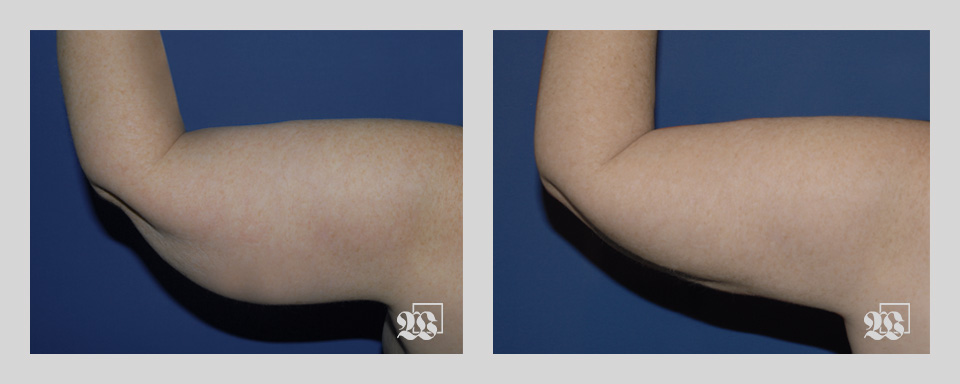
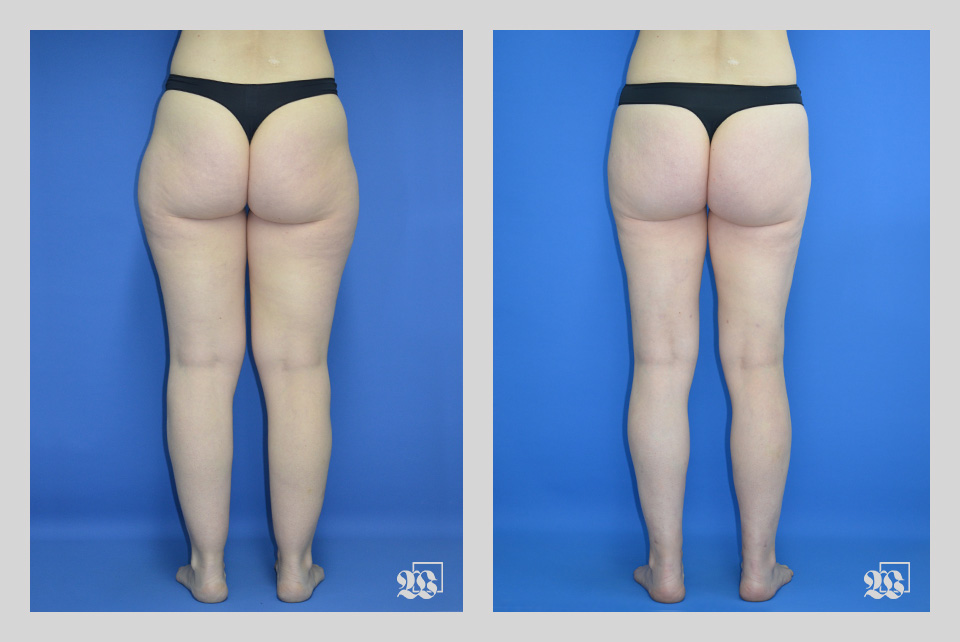
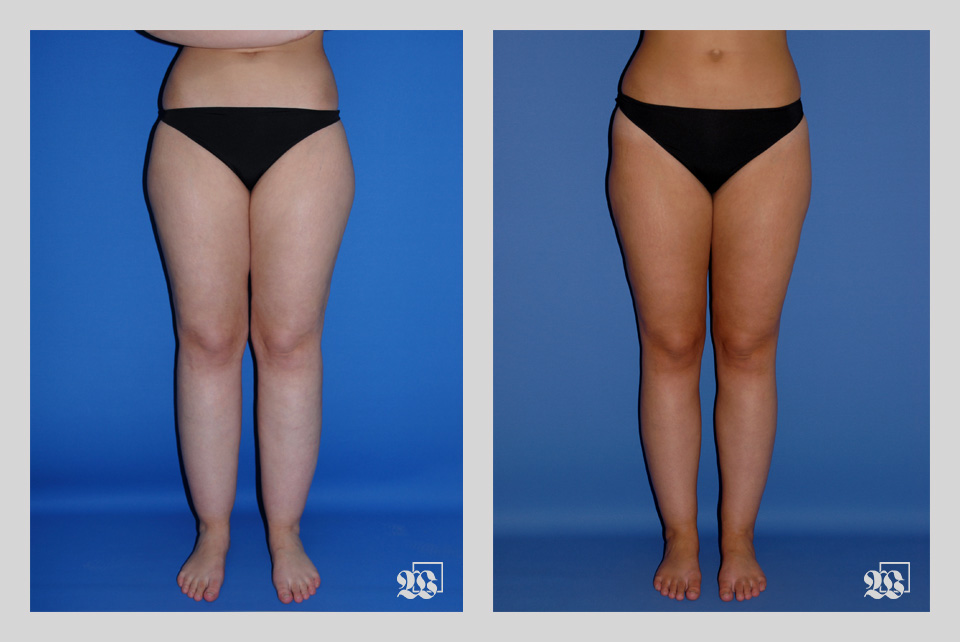
Patients suffer for years and feel their quality of life is markedly impaired. This is a result both of the appearance and the discomfort. The body image is disproportionate, as the women often have a thin or normal upper body but thick heavy legs and sometimes upper arms. In addition they suffer from the swelling and tenderness especially during warm weather, after prolonged sitting or standing and in the evenings.
How can I recognize the disease?
The most obvious feature – especially in young women of normal weight – is a disproportionate relationship between a thin upper body and a heavy lower body. The legs seem as if they belong to another body. There may be striking differences in clothing sizes; a patient may wear a medium blouse and extra large pants. Thus lipedema can be clearly distinguished from obesity and the symptoms also separate it from an unattractive distribution of fat, as seen in women with prominent „saddle bags“ on their thighs. The changes are always symmetrical. They can extend from the hips to the ankles, but often the legs are affected only above or below the knees, or arms and forearms may be involved. The excessive fat can be uniformly distributed over the entire leg producing so-called „piano legs“. The feet are invariably spared, so there may be a sharp transition around the ankles. In untreated patients, the condition slowly worsens. The skin and connective tissue become stretched and softer, so that the edema becomes more prominent and troublesome. Eventually the lymphatic system which helps return fluid from the tissues is damaged and drainage impaired so that secondary lipo-lymphedema evolves. In this advanced stage, the feet may also be affected by swelling. Corrective therapy by liposuction is no longer possible when this point has been reached.
Who gets lipedema and when?
Lipedema only occurs in women. It usually starts after puberty or during pregnancy. Lipedema patients may experience worsening while pregnant. The exact cause is unknown, but hormonal factors clearly play a role. Sometimes in a family nearly all females are affected, which suggests a genetic predisposition for the disorder.
Actual publication on this topic:
DERMATOLOGIE PRAXIS 2023; Vol. 33, Nr. 3
Stage 1 Skin surface relatively smooth, thickened fat layer, fine nodular fat structure
Stage 2 Skin surface uneven, coarse nodular fat structure
Stage 3 Folds of excessive skin and fat flaps/bulges, tissue coarse and hard palpable, transition to elephantiasis

How is lipedema treated?
Lipedema does not respond to diet or increased physical activity. Patients should try to maintain or achieve a normal weight, since being overweight is a risk factor for a worsening or a transition into lipo-lymphedema. Manual lymphatic drainage and the regular use of compression stockings (Class II-III) help reduce the symptoms of lipedema. The best way to permanently improve the problem is to remove the excess fat with liposuction with fine vibrating cannulas in local tumescent anaesthesia. This technique makes it possible to simultaneously remove 85% of the fat in a given area while sparing the lymphatic vessels. Clinical follow-up over up to 8 years shows that all patients achieve marked improvement in body contours, have fewer symptoms and enjoy a higher quality of life. These recommendations are reflected in the current German guidelines for lipedema. These recommendations can be found in the current guideline: PDF
How is liposuction performed?
Liposuction under local tumescent anaesthesia using fine vibration-assisted cannulas is a low-risk procedure which makes possible the permanent removal of excessive fat. The vibrating cannulas shake and loosen the fat cells from their attachments to the connective tissue without damaging the associated lymphatic vessels, blood vessel and nerves. The fat cells are then removed by suction.
The first results are clearly visible 24 hours after the procedure. One can begin to recognize about how the tissues will appear after healing. The fat cells which are both too large and too numerous are removed and do not regenerate. Two days after the procedure, minimal swelling appears as part of wound healing. Manual lymph drainage and the regular use of compression stockings speed the healing process in the first weeks. The long-term results can first be evaluated after 6 months, while the complete healing process takes another year. However, after just a few weeks the patient notices improved contours, fewer symptoms and a better quality of life. What an improvement!
LipödemZentrum Zentralschweiz LZZ – LipedemaCenter Central Switzerland
The LipödemZentrum Zentralschweiz LZZ offers its patients the entire diagnostic spectrum with state-of-the-art technical equipment under one roof at the Hirslanden Klinik St. Anna in Meggen. The conservative treatment options include Complex Physical Decongestive Therapy (CPD), Apparative Intermittent Compression (AIC) and individually appropriate compression garments, flat-knitted merchandise. Care is provided by specially trained and experienced professionals. Surgical therapy using vibration-assisted liposuction under tumescent local anaesthesia takes place in the operating rooms of the Hirslanden Klinik St. Anna in Meggen, using the highest level of professional expertise and under inpatient conditions.
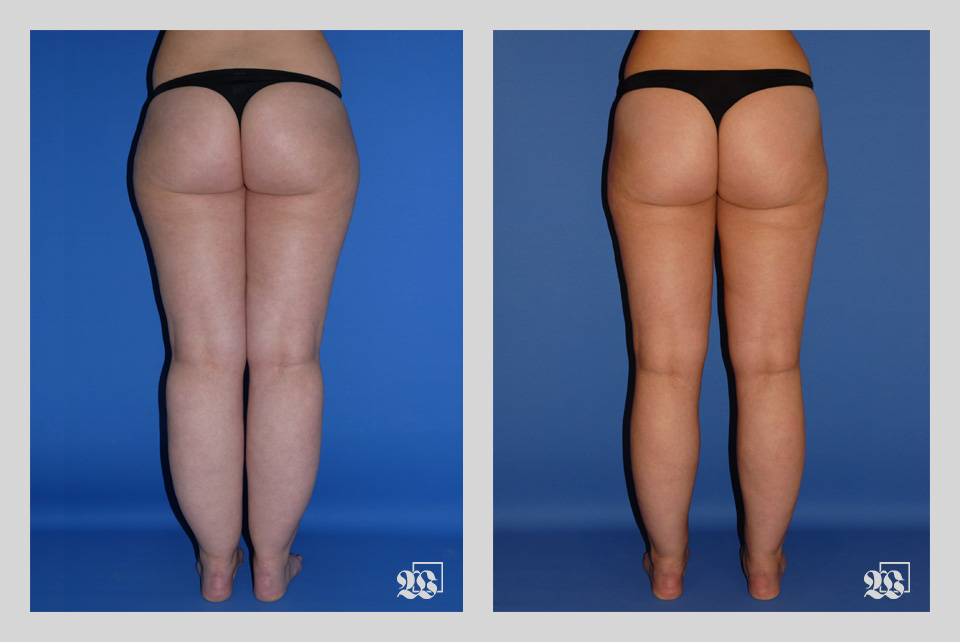
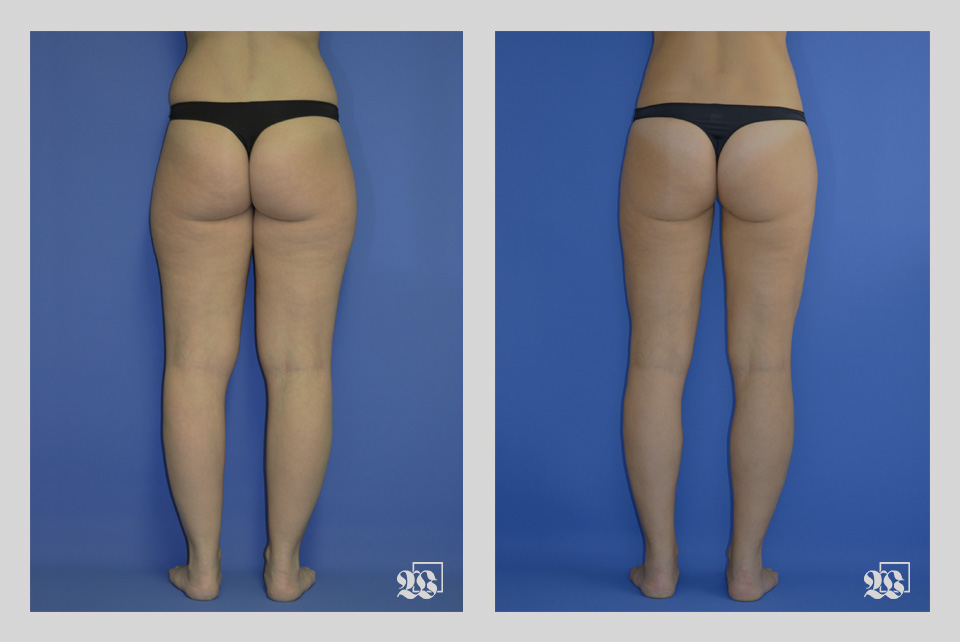
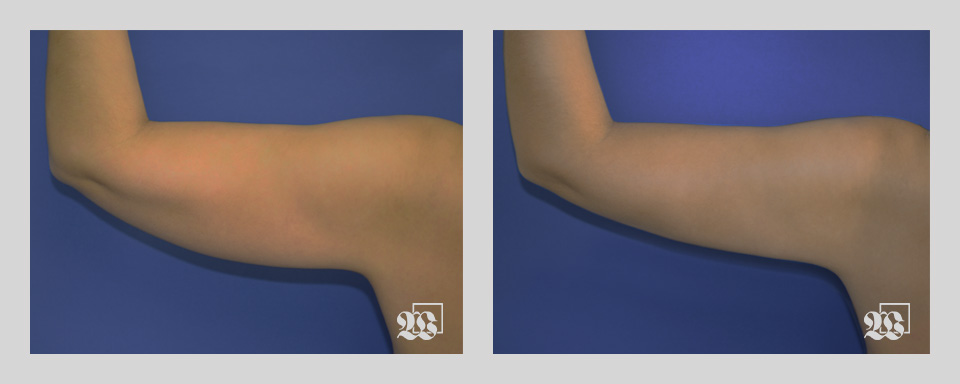
Patient 1

Patient 1
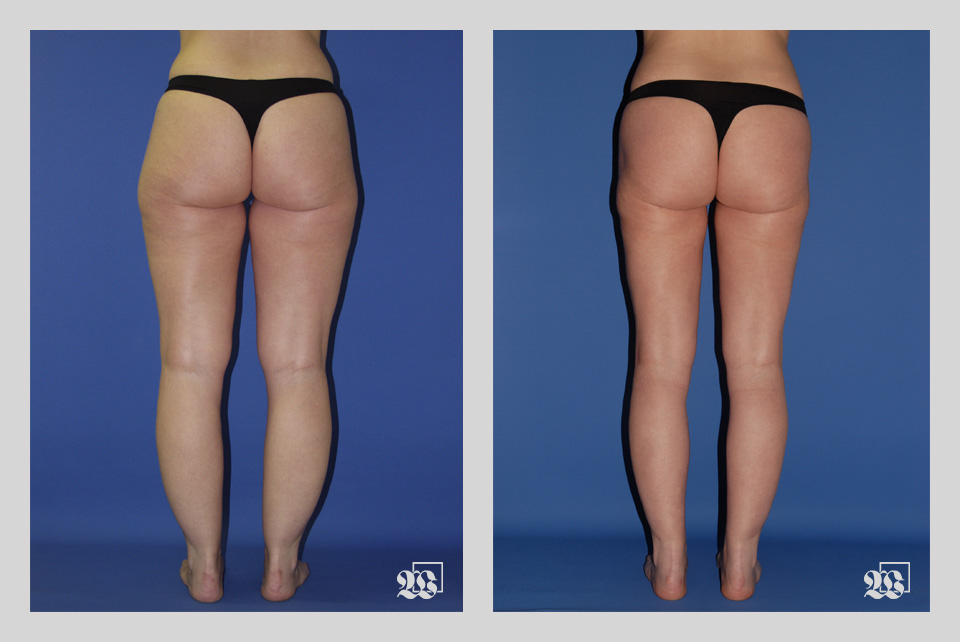
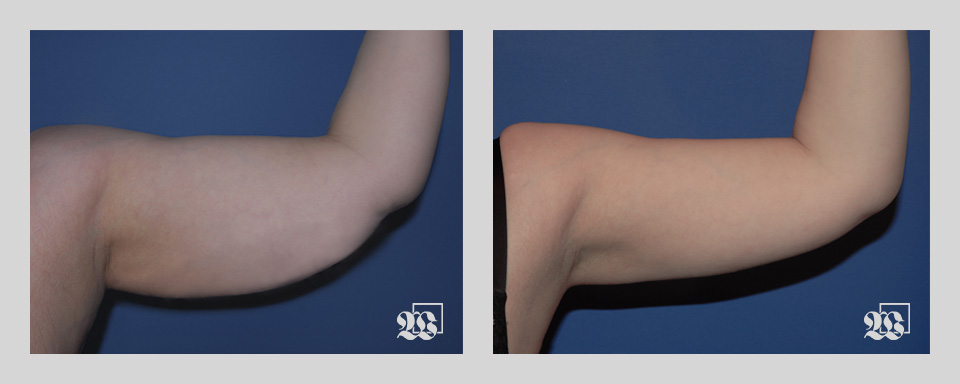
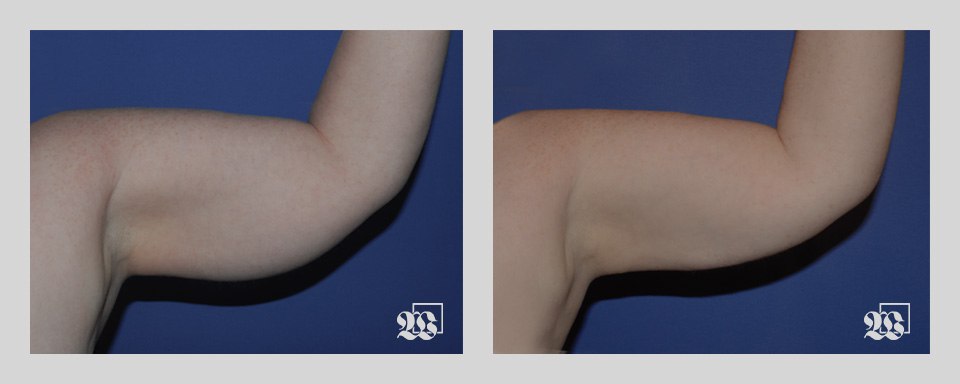
Patient 2
Patient 2
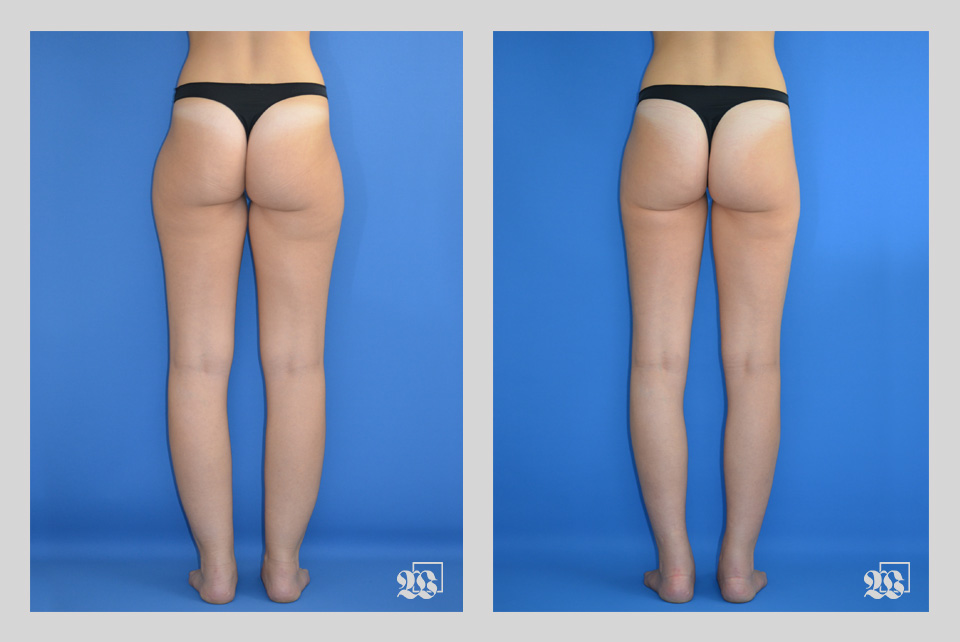
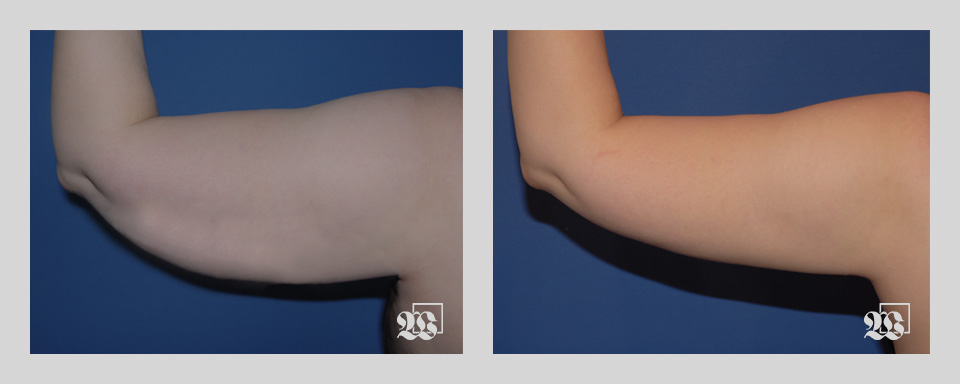
Patient 3

Patient 3
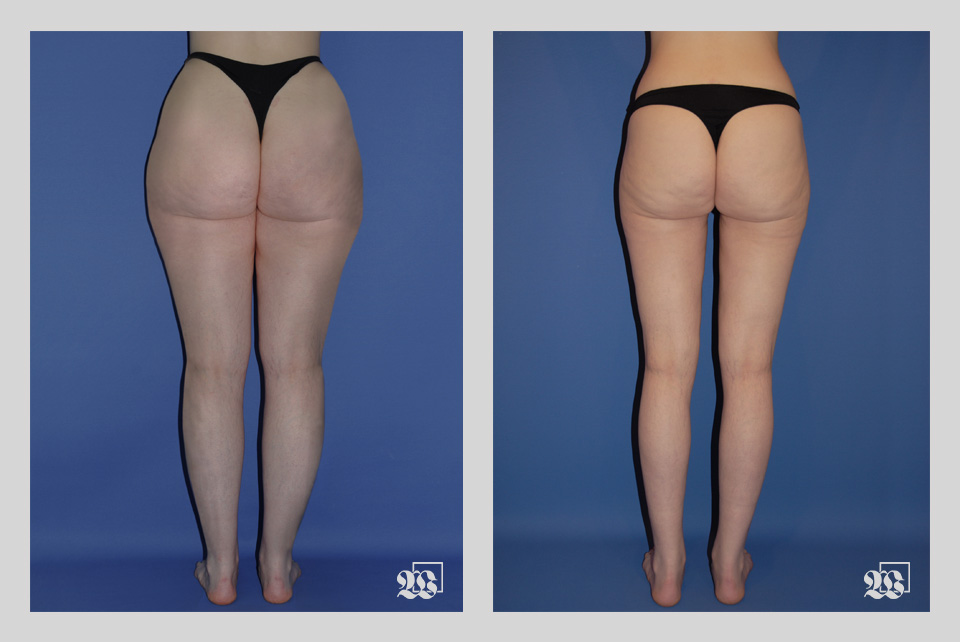
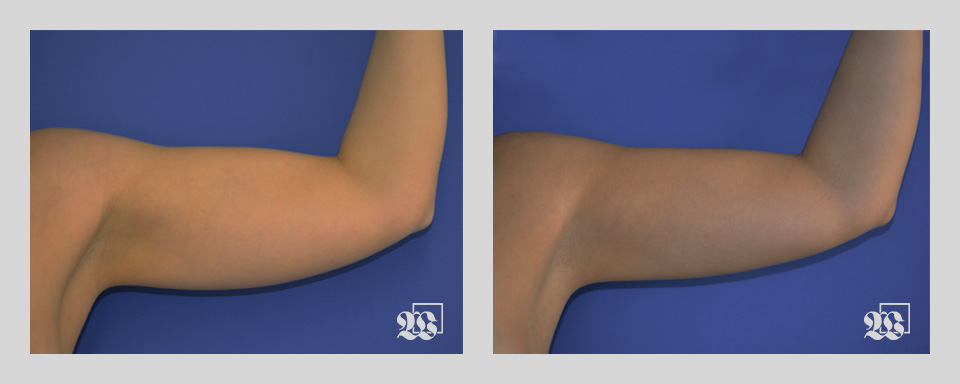
Patient 4

Patient 4
Patient 5

Patient 5
Patient 6

Patient 6

Patient 7

Patient 7
Patient 8

Patient 8

Patient 9

Patient 9

Patient 10

Patient 10

Patient 11

Patient 11

Patient 12
Patient 12
Patient 13
Patient 13
Patient 14
Patient 14